If you’ve seen one Medicaid agency, you’ve seen … One. Medicaid. Agency.
That’s one of our favorite sayings around here because it rings so true. Medicaid agencies are often assumed to be carbon copies in how they handle payment methodologies and other reimbursement matters, but nothing could be further from the truth.
The Medicaid agency in each state has quite a bit of flexibility and autonomy when it comes to reimbursement. They use various algorithms for how to reimburse, as well as updating published rates at varying frequencies. And even though most agencies look to Medicare for guidance, some are relying on outdated information (by months or even years!) to make reimbursement decisions.
Discrepancies like these can cause major headaches for manufacturers and providers alike, not to mention nightmare scenarios for patients struggling to get access to treatments they desperately need. It’s hard to blame providers who stop prescribing treatments that leave them “underwater” due to sometimes severe under-reimbursement. Not only does this present financial problems for the provider, but it can also lead to devastating gaps in treatment for their patients as alternative products are pursued.
Our advice? Making sure Medicaid reimbursement rates are in line from the start is the best way to go.
Let’s see how this plays out in action.
One of our clients had an oncology product in the market for a few years when they got wind of providers selecting alternative products due to under-reimbursement. DKP conducted a historical Medicaid pricing analysis and identified more than 30 states with fee schedule rates well below Medicare’s Average Sales Price (ASP).
After reaching out to the right people at the different Medicaid agencies, we were able to share up-to-date pricing information and discuss options for resolution. If this work led to even one patient getting the treatment they need, we call it a win.
So, who’s underwater?
Medicaid Fee Schedule Rate Vs. Medicare’s Average Sales Price (ASP) + 6%
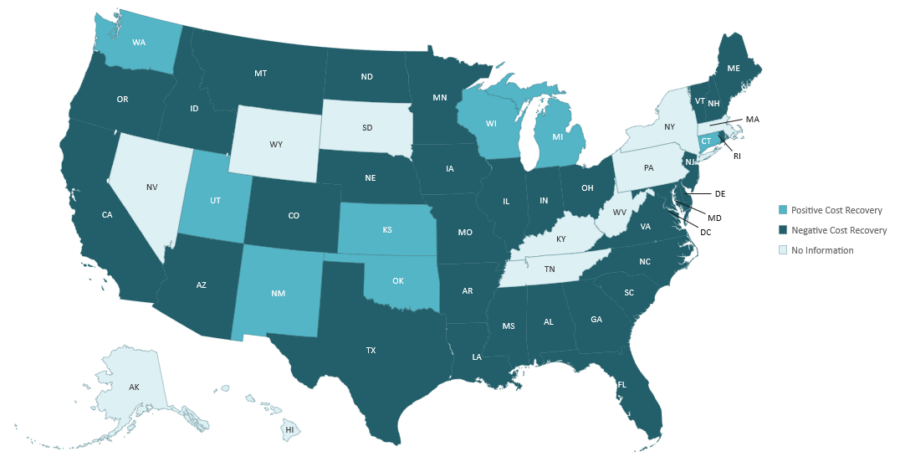
Here’s what we found: 32 states were under-reimbursed. And in some instances, states were being under-reimbursed by more than $2000.
That’s a lot of money left on the table (and not a big confidence boost for prescribers).
In addition to oncology products, we’ve also seen reimbursement nightmares play out in big ways in the cell and gene therapy and rare disease spaces. Novel therapies can carry hefty price tags from thousands to even millions of dollars per treatment. Medicaid agencies are continuing to work out guidelines for covering these first-in-class products while patients with catastrophic conditions wait in the wings. We’re watching closely as innovative reimbursement patterns are emerging and precedents are being set.
No matter the disease, no matter the product, no matter the price—what’s at stake most here is the patient’s chance of surviving and thriving. This is what drives us every day at DKP. It’s what we live and breathe. And Medicaid analysis, business intelligence, and outreach is just one way we do it.

